ASIS & AIIS Avulsion Fractures in Youth Athletes
Avulsion fractures of the anterior superior iliac spine (ASIS) and anterior inferior iliac spine (AIIS) are overuse or acute traction injuries of the pelvis most common in adolescents and young athletes. These injuries typically occur during rapid sprinting, kicking, or change of direction, and are seen often in soccer, track, baseball, and football.
What Are ASIS and AIIS Avulsion Fractures?
During growth, the pelvis has several secondary ossification centers (apophyses) where tendons attach to growing bone. In adolescents, these areas are weaker than the tendon itself.
- ASIS avulsion = avulsion of the sartorius (and partially tensor fascia lata)
- AIIS avulsion = avulsion of the rectus femoris (direct head)
When these muscles contract powerfully, the tendon can pull away a small fragment of bone from the apophysis—causing an avulsion fracture.
Mechanism of Injury
- ASIS Avulsion: Often occurs during sprinting, starting from a static position, or cutting
- AIIS Avulsion: Occurs during kicking, ball striking, or forceful hip flexion/knee extension
Seen most commonly in ages 13–17, particularly in males during growth spurts.
Symptoms & Clinical Presentation
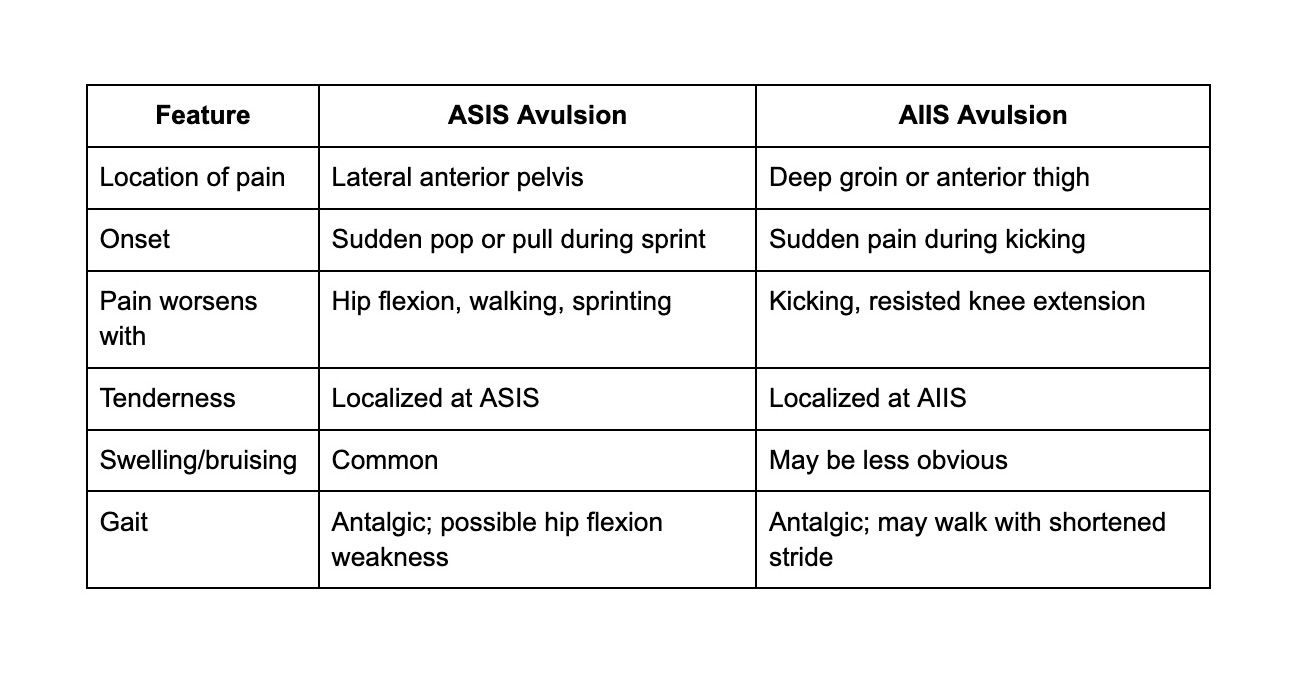
"Pop" or tearing sensation is commonly reported at onset. Swelling and bruising may take 24–48 hours to develop.
Imaging & Diagnosis
- X-ray (AP pelvis): Confirms bony fragment avulsed from ASIS or AIIS
- MRI or Ultrasound: Used when diagnosis is uncertain or to rule out tendon/muscle strain
- Important to differentiate from:
- Muscle strains (sartorius, rectus femoris)
- Apophysitis
- Slipped Capital Femoral Epiphysis (SCFE) in skeletally immature athletes
Non-Operative Management (Most Cases)
Indicated for fragments displaced <2 cm and no neurovascular compromise
Phase 1: Acute (Weeks 0–2)
- Relative rest + crutches for pain relief
- Ice, compression, and elevation
- No stretching or resisted testing of involved muscles
- Protected weight bearing (toe-touch to partial) as tolerated
Phase 2: Controlled Motion (Weeks 2–4)
- Wean crutches as pain allows
- Begin pain-free active hip and knee ROM
- Gentle isometrics for hip flexors and quadriceps
- Stationary bike (no resistance) if tolerated
Phase 3: Strength & Mobility (Weeks 4–6)
- Progress closed-chain hip/knee strengthening
- Core activation and gluteal strengthening
- Add eccentric work for hip flexors and quad strengthening
- Begin light sport-specific drills (e.g., low-speed running, soft tossing)
Phase 4: Return to Sport (Weeks 6–10+)
- Sport-specific sprinting, agility, and kicking drills
- Ensure:
- Pain-free with resisted testing
- Symmetric strength (90–95%)
- Normal stride and sprint form
- Return to competition when able to tolerate full intensity practice
Return to Sport Timeline
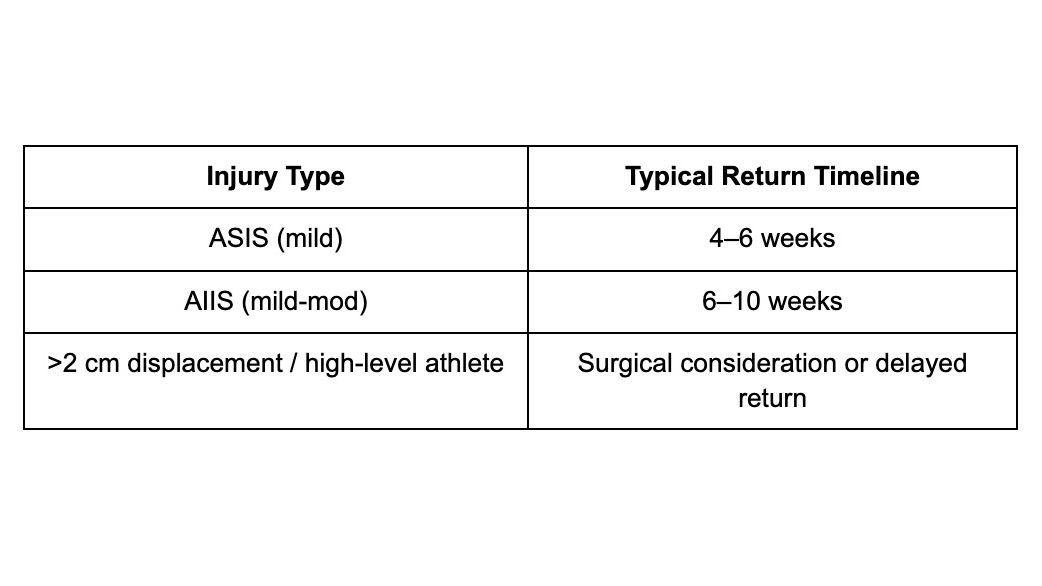
Surgical fixation is rare but considered if displacement >2 cm or nonunion occurs after 8–10 weeks.
Return-to-Play Criteria
- Pain-free sprinting, kicking, cutting
- No compensation or weakness on hip flexion or knee extension
- No tenderness on palpation
- Normal muscle length on flexibility testing (Thomas test, Ely's)
- Pass sport-specific simulation drills without symptoms
Athlete Education
- DO NOT stretch hip flexors aggressively early on
- Prioritize progressive loading, not early return
- Most return to full sport without complications with appropriate care
- Address asymmetries, glute weakness, and sprint form during rehab
References
1. Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001.
2. Kujala UM, Orava S, Karpakka J, Leppävuori J. Ischial apophysis injuries in athletes. Sports Med. 1997.
3. Sundar M, Carty H. Avulsion injuries of the pelvis in children: a report of 32 patients and a review of the literature. Pediatr Radiol. 1994.
4. Schuett DJ et al. Pelvic avulsion fractures: a retrospective review of 228 cases. J Pediatr Orthop. 2015.
5. de Sanctis N, et al. Avulsion fractures of the pelvis in adolescent competitive athletes: treatment and prevention. J Orthop Traumatol. 2003.
